Parametric optimization for medical devices
Nasal inhalers are common medical devices, they deliver a predefined amount of drug injecting it into the nasal cavity. Often, the medicine is a liquid which is reduced into small droplets by means of an atomizer, and in order to be correctly delivered, they must adhere to, and cross, the nasal cavity mucosa.
The quantity of medicine that is successfully administered to the patient (i.e. the quantity of medicine that sticks to the nasal cavity mucosa) is one of the fundamental aspects to be considered when designing these devices. And what makes the whole process challenging, is the fact that such quantity depends on many different parameters: the nasal cavity morphology (patient-specific), the injecting nozzle shape, the injection velocity, the inhaler position and alignment with respect to the cavity, the droplets size (mean and distribution), the injection start time with respect to the respiratory cycle are the main ones.
Typically, this issue is addressed using experiments: clinical trials or injection tests inside hand-crafted complex prototypes mimicking the nasal cavity. Both these solutions have significant drawbacks, like costs, repeatability, safety and so on.
A notable alternative is represented by virtual simulations: mathematical models able to reproduce physical behavior of air flows and dispersed particles are used to investigate in detail what happens, for each timestep, in each portion of the computational domain. This success story shows how Artificial Twin | PhyMo™ has been used for this exact purpose: using nasal cavities CAD models of different patients, the total drug deposition, for a given mass of medicine, has been optimized with respect to droplets size and injection angle. Whilst the complete study cannot be disclosed for confidentiality reasons, a single simulation result is reported below, allowing to completely grasp the power of this tool in performance optimization for medical devices.
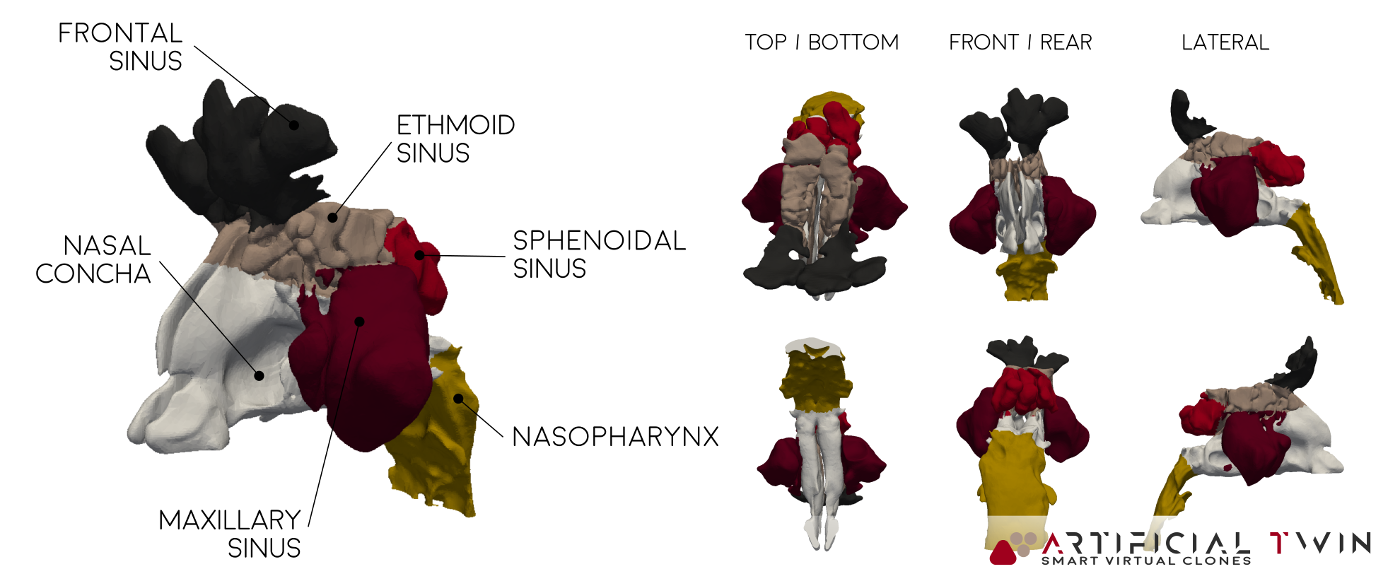
MRI-based, patient-specific, nasal cavity CAD model
In order to simulate what happens inside the nasal cavity, a CAD model reproducing it is needed. To reconstruct internal organs in 3D is a complex process, done in multiple steps. First a fine size MRI is needed, it basically provides a set of ordered sections. Then, with a dedicated software, these sections are linked one another to recreate a complete 3D geometry.
The nasal cavity CAD file used as input to obtain the simulation results shown in this page is represented in the image above. The classical shape can be recognized, and specific zones are differentiated using colors. This differentiation is reflected also on the deposition analysis: in order to have a better understanding of what is happening inside the domain, the deposition percentage is calculated separately for each zone, as will be shown later.
One additional note should be added for completeness: the nasal cavity CAD file usually undergoes some additional processing, in particular near the nostrils, to correctly take into account the inhaler geometry (which affects the flow field near to it) as well as to appropriately model the so called “inlet boundary”, where the air enters the domain (typically represented as a spherical surface few centimeters wide, with its center located on the nostrils center).

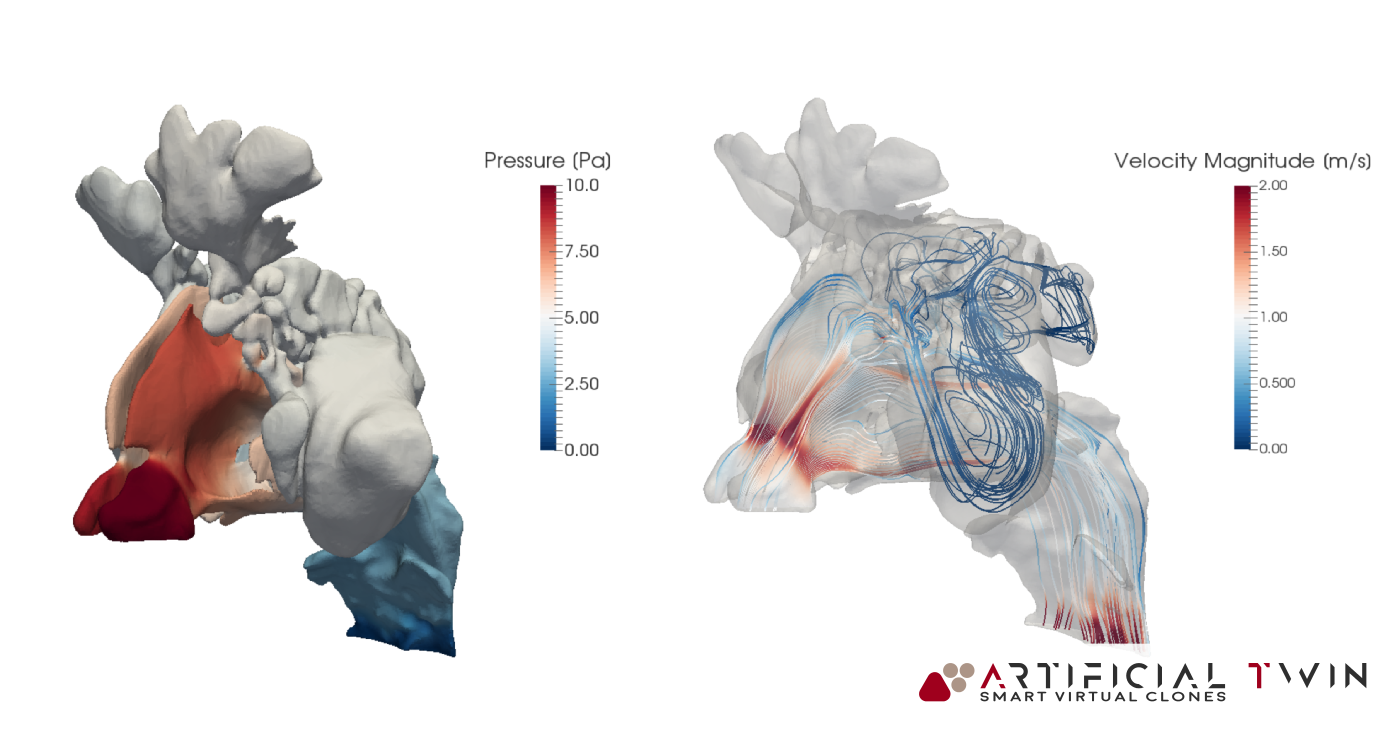
Simulation Pt 1: the airflow
With the CAD ready, the complete simulation workflow can start. It can be divided into two, conceptually independent, parts: one related with the airflow and one involving particles.
The very first step is the creation of the computational grid: the domain is discretized into small elements, called cells, where all variable values are calculated. Artificial Twin | PhyMo™ provides a very robust meshing tool, able to effectively handle very complex geometries, as in this case.
The first part of the simulation is focused on the airflow, it deals with calculation of all fluid dynamics variables, such as pressure, velocity and turbulence, resulting from the imposed boundary conditions. Results shown here represent a case where a steady, 5 seconds long inspiration is simulated. Of course, with proper setup, unsteady, transient flows can also be calculated, like a complete inspiration-expiration cycle.
In the images above and on the left it is possible to see some typical insights one obtains from this first part of the analysis: pressure distribution on nose cavity walls and flow lines (above) provide a 3D information, highlighting where narrow passages cause the velocity to increase and separate high pressure zones from low pressure ones. Nasal cavity sections (left) are a collection of 2D velocity magnitude contour maps, showing in detail what happens in twelve, equally spaced, slices of the domain.
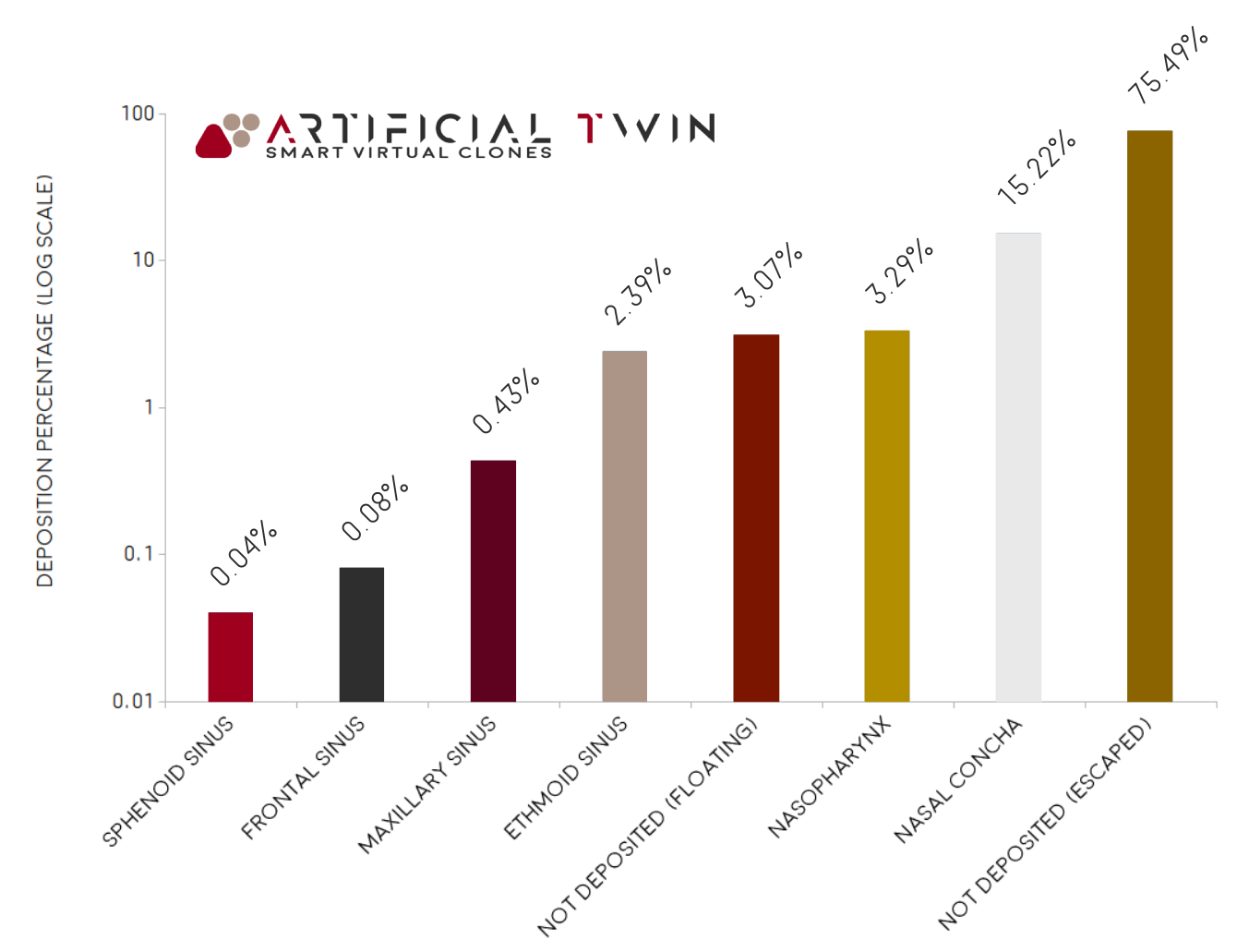
Simulation Pt 2: drug particles
The second part of the simulation involves dispersed particles motion. This Artificial Twin | PhyMo™ advanced functionality receives specific inputs characterizing particles, like the mass to be injected, their size in terms of mean value and distribution (uniform, normal, Rosin-Rammler, etc) and their density, and computes the trajectory for each of them. The path they follow is influenced mainly by local velocity vector, aerodynamic force acting on them, gravity vector and collisions with other particles and/or surfaces.
Particles injection can be specified in many different ways, from manually prescribed particles positions, to surface-related or cone-shaped bounded ones. In addition, it is also characterized by injection velocity, instantly injected mass and injection duration. Results shown here have been obtained using surface related injection with an axial velocity of 1 m/s and an injection duration of 0.2 seconds.
Another fundamental aspect is the wall interaction model. In this case, all walls have been defined as sticky (where colliding particles stick), except for the inlet and outlet ones, which are open and let particles leave the computational domain.
In the chart on the right, one of the most important simulation insights is reported: it represents how the total injected mass is distributed between deposited particles (about 22%), particles which left the domain (about 75%) and particles that, after 5 seconds, are still floating around (about 3%). Deposited particles percentage is itself divided between all nasal cavity zones, showing how a large portion of it (about 15% of the total 22%) deposited on the nasal concha, followed by nasopharynx and ethmoid sinus (about 3% and 2% respectively).
A complex optimization problem
The video on the right shows a complete animation where injected particles flow through the nasal cavity, coloring in blue those which sticks to walls and in red floating ones. It allows to qualitatively understand typical particles path and deposition zones, very valuable data practically impossible to obtain without virtual tests.
This type of study is highly complex and involves a large number of factors. For this specific case, in order to optimize the drug deposition percentage, a relevant number of parameters have been taken into consideration, resulting in a high dimensional search space.
Virtual simulations are very advanced tools, able to provide insights not available otherwise. As in this context, they play a key role in many others, driving designers intuition and creativity towards optimal, virtually tested, solutions.

